Talking T Cells

Professor Sheena Cruickshank on how the unsung stars of the immune system protect us against variants of SARs-CoV-2 and are the target of new vaccines for COVID-19 and AIDS
February 22nd 2022
Sheena Cruickshank is an immunologist and professor in biomedical sciences and public engagement at The University of Manchester. During the pandemic, she has been working with the UK Covid Immunology Consortium (UK-CIC) and helping explain to the public what we know about how the immune system responds to SARs-CoV-2 and COVID-19 vaccines.
She is particularly interested in the role of T cells in immunity. This complex group of differentiated white blood cells are involved in killing pathogens and infected cells, remembering previous infections, and support the production of antibodies.
Cruickshank, recovering from COVID-19 herself, spoke to The Biologist about why antibodies rather than T cells took centre stage for most of the pandemic and vaccine roll out, and how a new generation of vaccines that focus on targets to stimulate T cell responses should be able to offer better protection against variants of SARs-CoV-2.
Firstly, can you tell me what you've been up to over the course of the pandemic, and how your research has been affected by it?
It was very challenging trying to do research when our labs were shut down for such a long time, but we had a double whammy – when our labs finally reopened there was an electrical fire in our building, and we lost tens of thousands of pounds’ worth of kit. We couldn't really go in and rescue things properly because we were in lockdown measures.
Keeping your groups feeling motivated and happy has also been a real challenge for a lot of research groups. You have to try and keep everybody moving in a positive direction while also looking after your own wellbeing. A lot of people, myself included, are still struggling with either COVID or long COVID, or we're struggling with the ongoing drama of COVID in the house, and I think women have been disproportionately affected.
On the positive side, people have really embraced working across disciplines a lot more, and I think it's really brought to the forefront how important it is to engage with the public, policymakers and the media, to make sure that the right information is getting out there.
We've never seen this speed of information and content going up online, and a lot of misinformation and confusion. That's been one of my big focuses, to see how I can help to make sense of the latest COVID research in digestible ways. I thought that was that was one of the most useful things I could do.
The role of T cells seems to have come to the fore only recently, amid concerns that the Delta and Omicron variants could evade the antibodies generated by COVID-19 vaccination. Firstly, can you explain what T cells do that gives us this broader and longer-lasting defence compared to antibodies alone?
The thing to understand is that the immune system has different ways to deal with an infection – it is an overlapping, multi layered system, and there are lots of components that are all doing things that complement each other. You've got two main flavours of lymphocytes: B lymphocytes, or B cells, which are the ones that can make antibody, but you've also got T cells or T lymphocytes. Cytotoxic T cells, or killer T cells, basically blast holes in infected cells and they can produce products that stop viruses replicating or kill them. So, they're very, very effective at killing.
There are also helper T cells, which do as you'd imagine: they help things. So, they help B cells make antibody, and they can also help cytotoxic T cells do the killing. They're absolutely crucial cells – probably the most important immune cell type in our body.
The T helper cells, the cytotoxic T cells, and the B cells are all working together so you need all these cells for the best immune response. A virus has lots of different features on it, and both the B cells and T cells will be looking for unique features to target. The B cells essentially see shapes, and tend to react to things on the virus surface. But the T cells don't see shapes – they target sequences of amino acids found on or in the virus. There is evidence that they're also seeing things inside the virus, not just things on the outside, such as factors that are involved in viral reproduction.
So we have this breadth of immune response, with lots and lots of targets that these immune cells can recognise, which reduces the chance that you're going to get viral evasion.
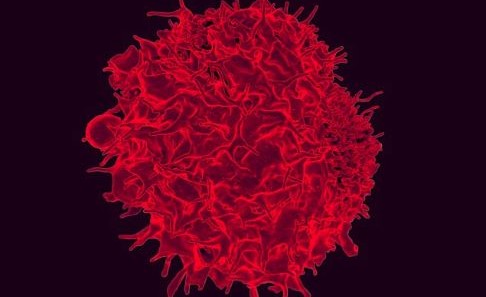 A colorized scanning electron micrograph of a T lymphocyte. Credit: NIAID
A colorized scanning electron micrograph of a T lymphocyte. Credit: NIAIDAnd so even when the number of SARs-CoV-2 specific antibodies has dwindled to virtually nothing, a level of T cell immunity remains.
Over time that you tend to get cells that dominate, depending on the stage of the infection. So, in coronavirus infection, antibodies seem to be primarily trying to stop the virus from getting into our cells. When you have the initial immune response, you have this peak where lots of antibody is being produced, lots of effector molecules are being produced from the T cells, but that will go down over time – you really don't want that to stay up very high or you could get damage to your body.
We have a period of ‘protective immunity’ where, for example, you might have antibody levels that will be enough to start dealing with the infection immediately. But you will also have memory, so you'll have B memory and T memory cells. When B memory cells get prompted again with that same virus, they will start making more of the plasma cells that make antibody, the T cells will start making more of the cells to kill and helper cells to help make antibody. Those memory cells, whether the B or T cells, last a very long time – as long as 90 years!
Plasma cells are the type of B cell that can make antibody, and for some infections they will persist so that you'll always get a little bit of that circulating antibody. That is not happening in COVID, and hence why sometimes antibody levels can drop right off. Whether that's because we've not got the formulation of the vaccines quite right or whether it's something about the nature of the disease I’m not sure – I suspect it's the latter because this is something we've seen with other coronaviruses before and we don't entirely know why.
So unfortunately, we don't seem to have long lived antibodies in everybody. But, if you've got a good memory T cell response, that seems to be very helpful for trying to help your B cells and long-lived plasma cells make new antibodies.
You mentioned other coronaviruses there. What do we know about whether T cell memory of other beta coronaviruses can help us fight off COVID?
Quite early on in the pandemic there was evidence of people having antibodies and T cells that recognise bits of SARS-CoV-2. We can see that there are features that are common to some viral strains, and that's particularly true of things found within the virus such as reproduction and replication machinery. It was suggested that the reason children have done a little better in terms of their response to COVID might be something to do with the fact they get an awful lot of colds, as anybody who is a parent knows. Some of the cold viruses are types of coronaviruses. There's also some crossover between some of the features of spike protein between SARS and SARS-CoV-2 – there seems to be quite a bit of a similarity there.
So the idea is that having lots of colds and having had them recently could be a factor in giving children a level of immunity or a level of protection against SARS-CoV-2?
Yes, it's like your immune response needs a little bit of a reminder. If there's enough similarity to the way that they've recognised a recent virus, and they keep getting it, that will always give the immune system a little prompt so that it never quite forgets.
So given that we have this complex, intricate immune response, is it fair to say that, even among infectious disease specialists, too much emphasis has been placed on antibody response during the pandemic?
I think there's lots of things that underlie that. So firstly if you want to do rapid assays for lots and lots of people across the world, antibody is much, much easier to measure. There are of course different assays to measure T cells and B cells, but antibody gives you a really useful and rapid fingerprint, whereas T cells require you to do quite involved assays, and there is no way around that unfortunately.
Scientists were also trying to react very quickly to what was known about the infection. Once we knew the spike protein is how the virus gets into our cells, that was an obvious target to start with. Generally, you want to go for a simple target and you want to go for something that's quite robust across a big population.
As we've learned more about the virus and now we are getting evidence of cross-reactive immunity, we can start to redefine and reassess what's best to do. Also, as we're seeing the evidence of the declining levels of neutralising antibodies, again that makes us assess what we're doing.
Looking ahead to second or third generation vaccines to help us develop as broad a response as possible to prepare us for future variants – how are these vaccines being designed with T cell responses in mind?
These are already going into trial, some looking at single targets but most looking at a combination of targets. Instead of the surface proteins, the targets may be things that are found within the virus that allow us to interfere with viral replication.
I think the shift now that is happening now is understanding that perhaps we shouldn’t expect completely blocking vaccine, because we're not really seeing the evidence for that. I may be wrong, we may develop one that's going to be completely blocking and you can't get infected, a completely sterilising version. But it looks like what is happening with the current vaccines, and what we want in the future, is vaccines that stop us getting really sick and stop us from dying, basically to help us live with the infection. That's what the broader vaccines are going to be able to do, and potentially, they'll be more fit for purpose for any variants, because clearly we're going to keep getting variants. Like the immune response itself, it’s about not having all of your eggs in one basket.
So, a mix of targets but essentially the same vaccine platforms?
Yes, we're still looking at protein vaccines, mRNA vaccines and viral vector vaccines, but they might be what we call multi-valent, so they have more than one antigen target in them.
Beyond COVID, what other areas of T cell research do you find exciting?
There are loads of interesting areas of research – T cells are so important. Vaccines for diseases like AIDS are certainly being investigated, and another exciting thing that's already happening is engineering T cell responses to cancer cells. There's a lot of work happening there that involves helping your own T cells do a better job of dealing with your cancer. Also, understanding how T cells get switched off by cancer and overriding that, such as checkpoint inhibitor therapy, that's all really exciting and the more we know about that the better.
We are also looking at how we can reprogram T cells in other conditions. For example, in allergies, can we reprogram T cells to stop them from helping B cells to make immunoglobulin E in the presence of the allergen, which drives the activation of an immune reaction? There are T cells that go awry in all sorts of conditions, so again, can we reprogram or redirect their activity? Regulatory T cells can help calm inflammation down, so they are a really important target in lots of conditions, such as autoimmune diseases.
There's so much happening! T cells are also really good at fighting fungal infections – so can we make them work better? The more we know about all the intricacies of these different subsets of immune cells, the more we can look at tailoring more effective treatments to individuals. I think that this is all helping us to move to a more personalised medicine, where it really looks at your unique features and how you can do better against whatever you are fighting against.
Another thing to look at is if we can we make our T cells better as we age. Our T cell function tends to deteriorate as we age, so can we get them going again when they've stopped working well, or when we have chronic infections which can also make our T cells less effective?
And, presumably, that links back to COVID-19 and disease severity – if T cell activity is declining, that's why we're seeing older people suffering more severe illnesses?
Absolutely. We know that a whole host of different conditions – not just ageing, but also things like obesity, can affect the function of your T cells. So again, understanding that is a really big, big topic, and one that’s more and more important because we are an ageing population. Getting our T cells to work better and be fitter for longer would be brilliant.
Interview by Tom Ireland
Sheena Cruickshank is Professor in Biomedical Sciences and Public Engagement at The University of Manchester.